The Silent Alarm in Your Bloodstream
Imagine this: You’re in an important meeting when a sudden wave of dizziness, cold sweat, and confusion hits you. Or perhaps, for weeks, you’ve felt an unquenchable thirst, fatigue that coffee can’t fix, and blurry vision. These aren’t just bad days; they are your body’s desperate SOS signals. Every year, millions confuse the symptoms of low blood sugar (hypoglycemia) with high blood sugar (hyperglycemia), a mistake where the wrong action can turn a manageable situation into a life-threatening crisis. With diabetes affecting 1 in 10 adults globally and complications on the rise, this isn’t just medical information—it’s essential life knowledge. This definitive guide cuts through the confusion, offering you a clear, actionable roadmap to distinguish, address, and prevent dangerous blood sugar extremes.
Why This Guide? Understanding the Urgency
Why trust this guide? Because it’s built on a foundation of medical authority and stark reality. The International Diabetes Federation projects 853 million adults will have diabetes by 2050. More immediately, the CDC reports a 21% spike in diabetes-related ER visits in recent years, often due to preventable crises. This guide merges clinical expertise with actionable steps, transforming complex medical data into a survival manual for daily life. Your confusion ends here.
Blood Sugar 101: The Fuel of Life
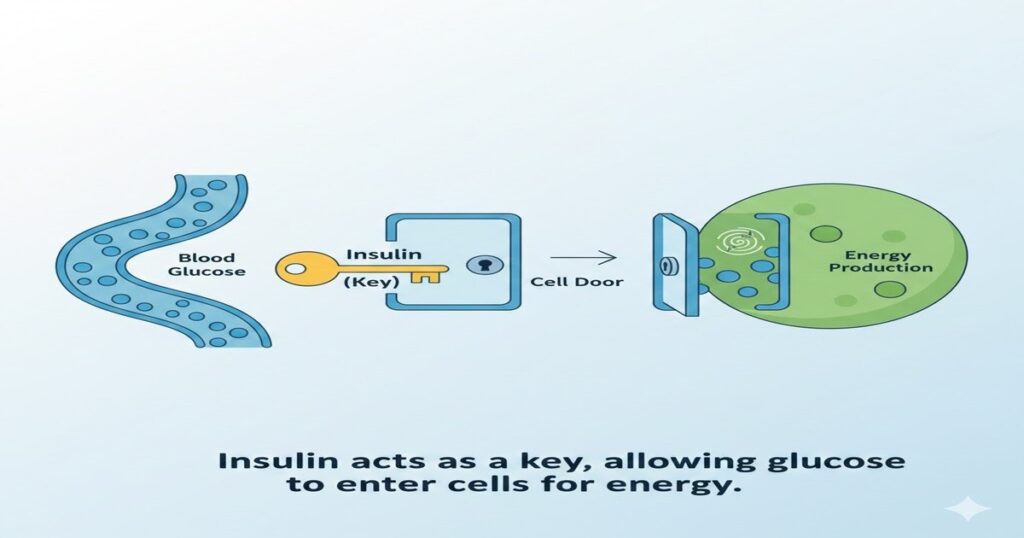
Blood glucose isn’t just a number; it’s the premier fuel for your brain and body. Insulin acts as the key, unlocking cells to use this fuel. In diabetes—Type 1 (autoimmune), Type 2 (lifestyle-influenced), or gestational—this system fails. Maintaining a level between 70-140 mg/dL is crucial; deviations trigger the symptoms we must learn to decode.
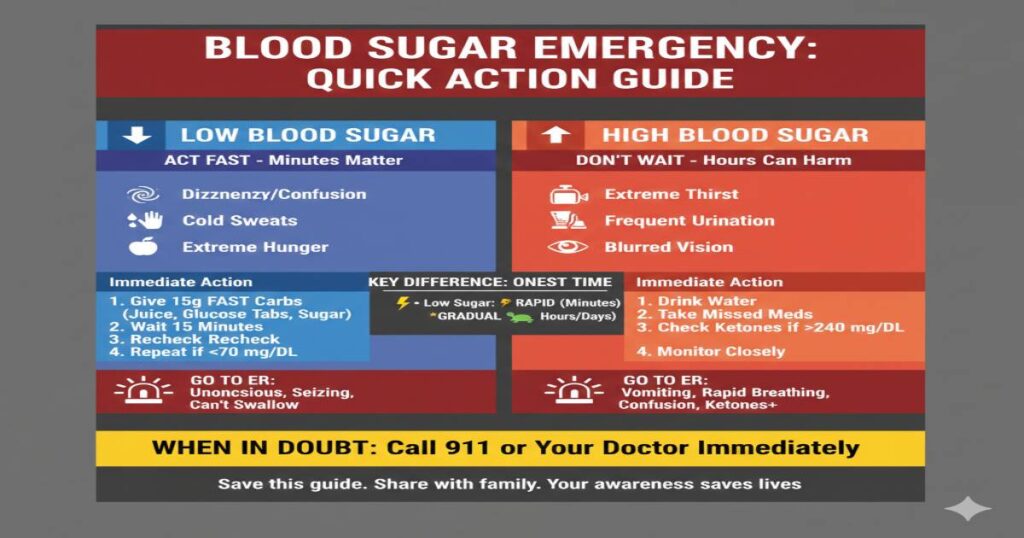
Side-by-Side Symptom Chart: Your Quick-Reference Lifesaver
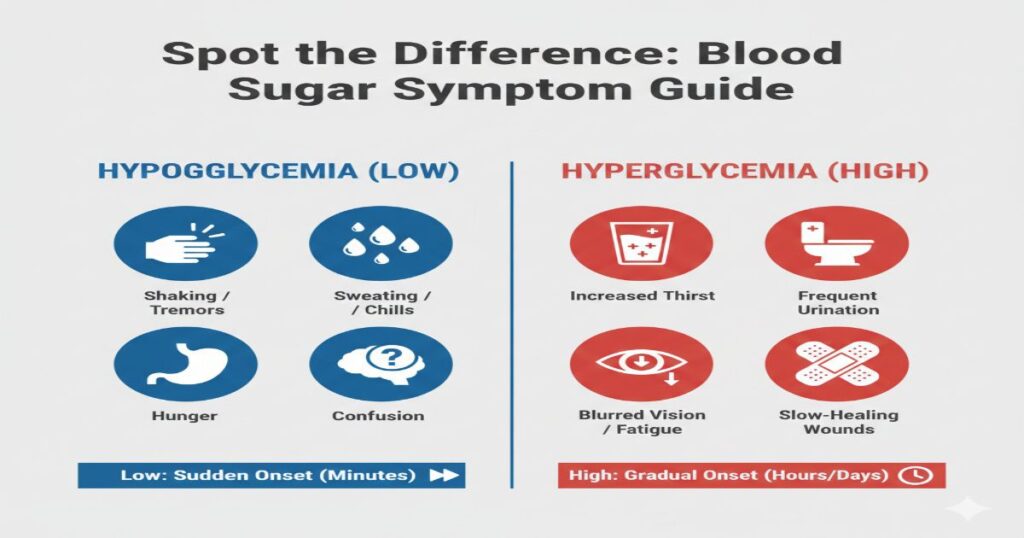
| Symptom / Sign | Hypoglycemia (Low Sugar) | Hyperglycemia (High Sugar) |
| Onset | Minutes | Hours to Days |
| Hunger | Ravenous, urgent | Loss of appetite |
| Sweating | Cold, clammy sweat | Dry, flushed skin |
| Neurological | Dizziness, confusion, irritability | Fatigue, difficulty concentrating |
| Physical Signs | Shakiness, palpitations | Increased thirst, frequent urination |
| Breath | Normal | Fruity smell (in DKA) |
| Critical Threshold | Below 70 mg/dL | Above 240 mg/dL (Risk Zone) |
Deep Dive: Hypoglycemia (Low Blood Sugar)
Causes & Physiology
Often a treatment side effect: too much insulin, skipped meals, unplanned exercise, alcohol.
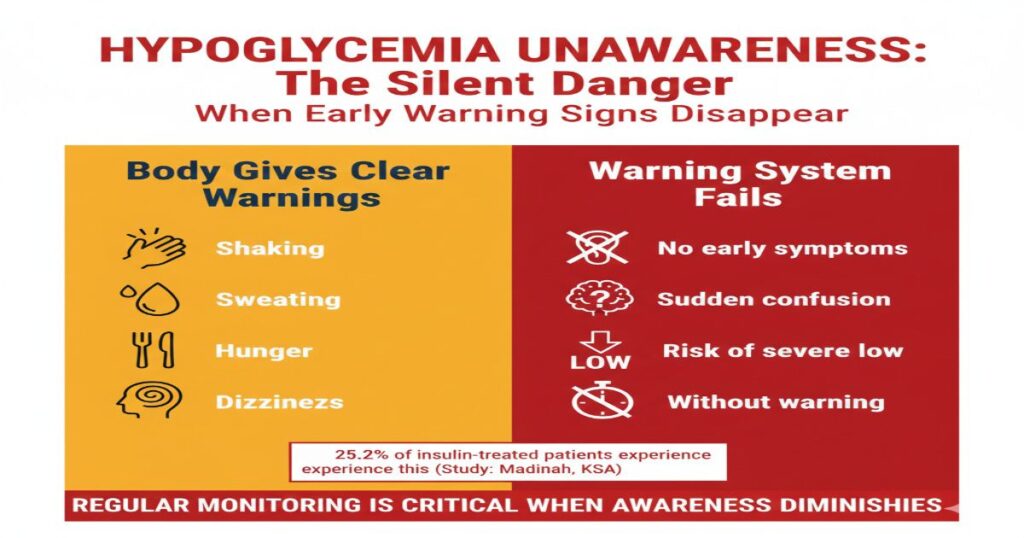
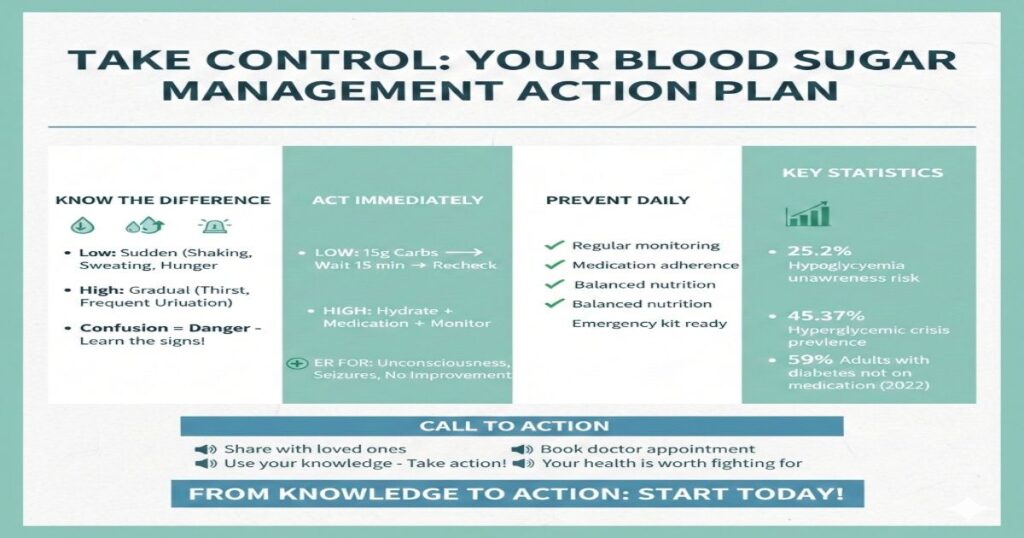
The Danger of “Unawareness”
A chilling 25.2% of insulin-treated patients lose early warning signs, risking sudden severe episodes.
Deep Dive: Hyperglycemia (High Blood Sugar)
Causes & The Stress Connection
Insufficient medication, dietary miscalculation, illness, and stress-induced cortisol release.
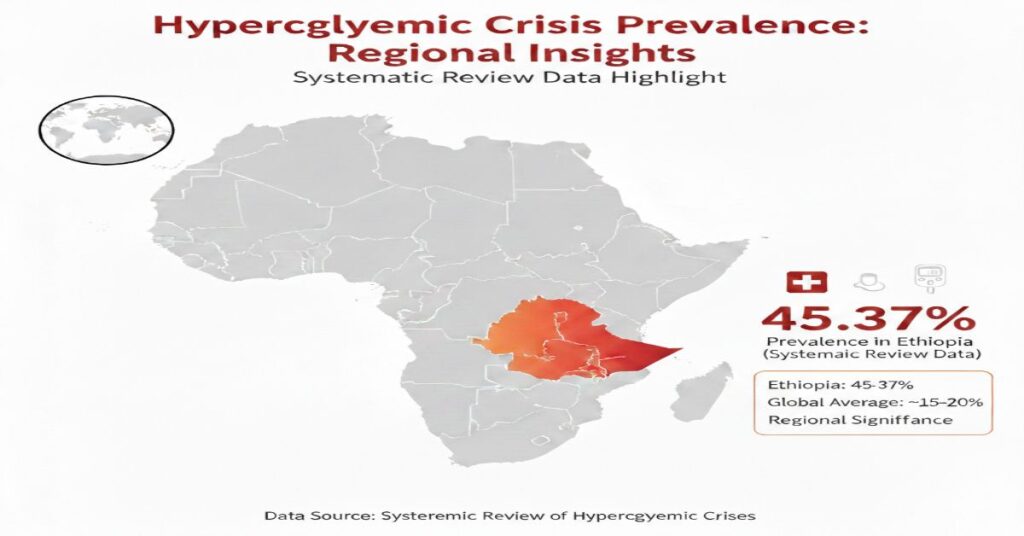
Statistical Reality Check
A systematic review found a 45.37% prevalence of hyperglycemic crises in Ethiopia, highlighting its global scale.
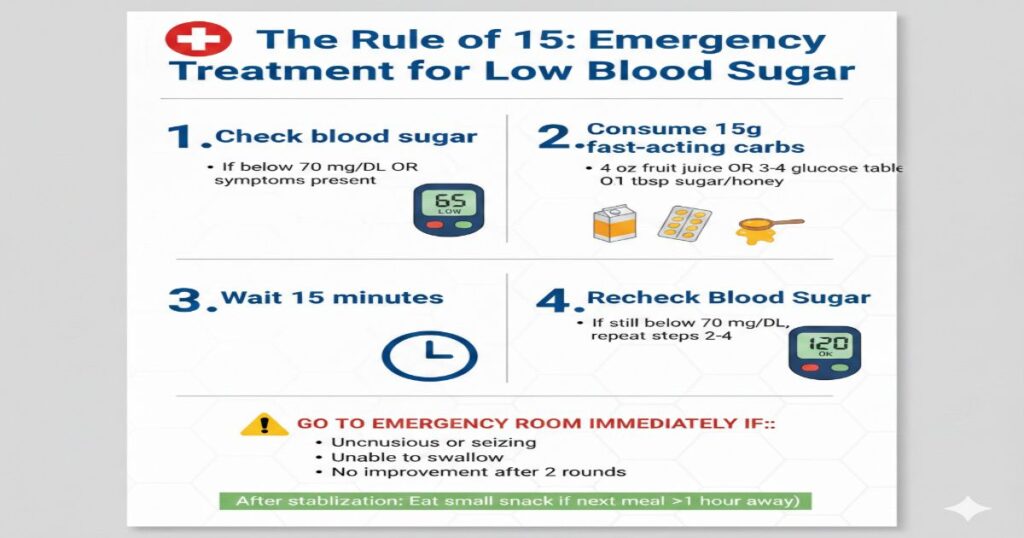
For LOW Sugar (The Rule of 15)
The Rule of 15: Emergency Treatment for Low Blood Sugar
Step 1: Check blood sugar
• If below 70 mg/dL OR symptoms present
Step 2: Consume 15g fast-acting carbs
• 4 oz fruit juice OR 3-4 glucose tablets OR 1 tbsp sugar/honey
Step 3: Wait 15 minutes
Step 4: Recheck blood sugar
• If still below 70 mg/dL, repeat steps 2-4
GO TO EMERGENCY ROOM IMMEDIATELY IF:
• Unconscious or seizing
• Unable to swallow
• No improvement after 2 rounds
After stabilization: Eat small snack if next meal >1 hour away
For HIGH Sugar
Immediate Actions for Hyperglycemia:
| Step | Action | Details |
|---|---|---|
| 1 | Hydrate | Drink water regularly (avoid juice/soda) |
| 2 | Medication | Take any missed diabetes medication |
| 3 | Monitor | Check blood sugar every 1-2 hours |
| 4 | Ketones | Test if blood sugar >240 mg/dL |
GO TO EMERGENCY ROOM IMMEDIATELY IF: • Vomiting or unable to keep liquids down • Rapid, deep breathing (like panting) • Confusion, drowsiness, or loss of consciousness • Blood sugar above 300 mg/dL with ketones present
Important: Contact your doctor if high sugar persists beyond 24 hours.
DKA vs. HHS: Decoding Critical Hyperglycemic Crises
| Condition | Diabetic Ketoacidosis (DKA) | Hyperosmolar Hyperglycemic State (HHS) |
| Blood Sugar | Above 250 mg/dL | Above 600 mg/dL |
| Ketones | High | Low/Negligible |
| Typical Onset | Faster (Hours) | Slower (Days/Weeks) |
| Key Risk Group | More common in Type 1 | More common in Type 2 |
Proactive Prevention: Your Daily Defense Strategy
Monitor: Use a glucometer or CGM. Data is power.
Adhere: 59% of adults with diabetes were not on medication in 2022—consistency is key.
Educate: Ensure your circle knows these signs.
Plan: Implement “sick day” rules—illness spikes blood sugar.

Frequently Asked Questions (FAQ)
Q1: What is the main difference between low and high blood sugar symptoms?
A: The core difference is onset and sensation. Low sugar hits fast with physical urgency (shaking, sweating). High sugar builds slowly with systemic distress (thirst, fatigue).
Q2: Which is more dangerous immediately, hypoglycemia or hyperglycemia?
A: Severe hypoglycemia is an immediate life-threat (risk of seizures, coma within minutes). Severe hyperglycemia (DKA/HHS) is a critical but slightly slower-onset emergency.
Q3: Can you have symptoms of both high and low blood sugar at the same time?
A: Not simultaneously, but you can experience “false hypoglycemia” where rapidly falling high sugar triggers low-sugar symptoms.
Q4: What is the “15-15 rule” and when should I not use it?
A: The Rule of 15 is for conscious, able-to-swallow individuals. DO NOT use it if the person is unconscious or seizing—use glucagon and call 911.Q5: How often should I check my blood sugar if I’m experiencing symptoms?
A: Check immediately when symptoms start. If treating a low, recheck every 15 minutes until stable. For unexplained highs, check every 1-2 hours.
Conclusion: Empowerment Through Knowledge
The flux between high and low blood sugar is more than a numbers game—it’s a daily dialogue with your body. Recognizing the sudden tremor of a hypo versus the creeping fatigue of a hyper empowers you to respond not with panic, but with precision. In a world where diabetes statistics can feel overwhelming, remember: knowledge is your most potent medication. This guide is your compass. Bookmark it. Share it with someone you love. Let it be the reason you catch a warning sign early. But let your final action be this: Take this information, partner with your doctor, and build a management plan that lets you live fully, confidently, and in control. Your health isn’t just worth reading about—it’s worth fighting for.
Disclaimer: This guide is for informational purposes and does not replace personalized medical advice from your healthcare provider.

